If you’ve been wondering whether Long COVID could affect fertility, you’re not alone. It’s a question many people are asking as they deal with lingering symptoms after COVID-19. We know that this virus doesn’t just hit hard during the acute phase—it can leave a lasting imprint on many parts of the body. Now, growing research suggests that both men and women may experience changes in reproductive health after infection. From irregular periods and hormone imbalances to sperm quality and libido, fertility may be one more area where Long COVID has a hidden impact.
Understanding the Connection Between Long COVID and Fertility
Long COVID refers to symptoms that persist weeks or even months after a COVID-19 infection. These symptoms often include fatigue, brain fog, and shortness of breath—but researchers are now investigating how Long COVID might affect reproductive health. Inflammation, immune dysregulation, and even direct damage to reproductive organs are some of the possible mechanisms. For example, studies have found that the virus can linger in the testes, possibly affecting sperm production (NIH). In women, menstrual irregularities and worsened premenstrual symptoms have also been observed (BMJ).
Male Fertility and Long COVID
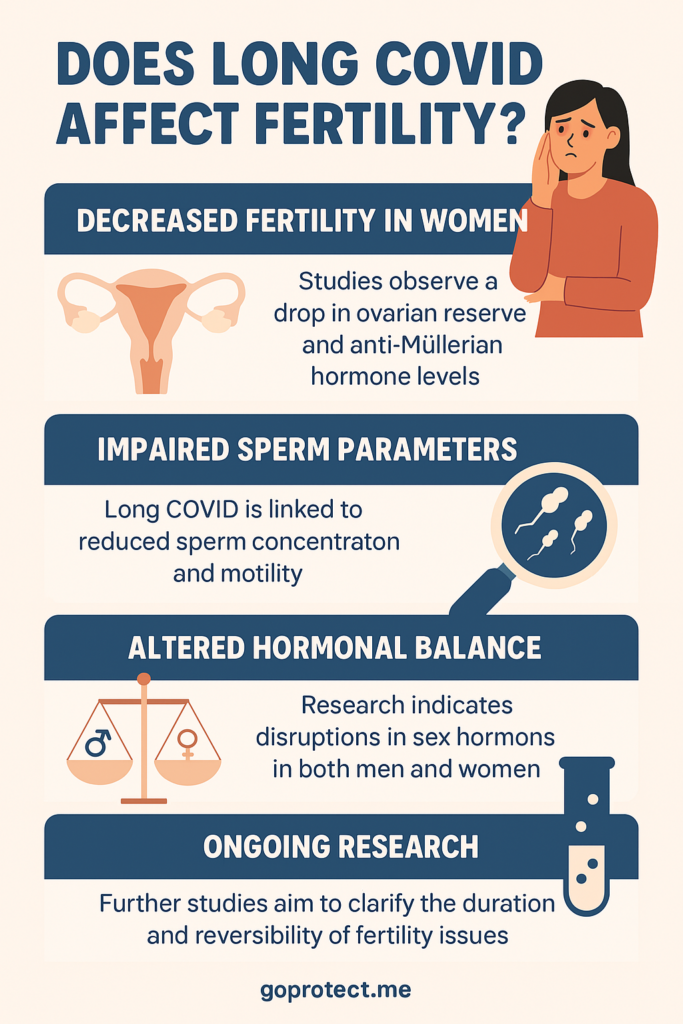
Several studies have pointed to a temporary drop in male fertility following COVID-19. A 2022 study published in Andrology showed reduced sperm count and motility in men who had recovered from COVID-19, especially those with moderate or severe illness (Andrology Journal). Long COVID may also contribute to hormonal changes that affect testosterone levels, which can influence sex drive, mood, and reproductive capacity. In some cases, the virus may cause inflammation in the testes (orchitis), further complicating fertility.
Female Fertility and Long COVID
Women have also reported changes in their menstrual cycles after COVID-19. According to a study published in The Lancet, some women experienced delayed or missed periods, heavy bleeding, or more severe cramps post-infection (The Lancet). These symptoms could be linked to inflammation, stress, or immune system disruption. While most cycle changes seem to resolve in a few months, ongoing research is investigating whether these alterations might affect fertility or reproductive aging in the long term.
Hormones and the Hypothalamic-Pituitary-Gonadal Axis
COVID-19 can disrupt the body’s delicate hormonal balance. The hypothalamic-pituitary-gonadal (HPG) axis, which regulates reproductive hormones, may be thrown off by systemic inflammation or stress related to Long COVID. This can lead to imbalances in estrogen, progesterone, and testosterone. Low estrogen can affect egg quality and uterine lining development, while low testosterone can reduce sperm production and libido. These shifts may not be permanent but can certainly affect fertility while the body is still healing.
Ongoing Research: What We Know So Far
Scientists are still in the early stages of understanding how Long COVID affects fertility. A large study funded by the National Institutes of Health (NIH) is currently tracking menstrual changes in over 20,000 participants to better understand the long-term effects of the virus (NIH Researching COVID to Enhance Recovery). Meanwhile, researchers at Mount Sinai are studying hormone levels and reproductive outcomes in both men and women with Long COVID to provide more concrete answers.
Natural and Holistic Fertility Support
If you’re navigating fertility challenges after Long COVID, there are holistic ways to support your reproductive health. Eating an anti-inflammatory diet rich in omega-3s, leafy greens, and whole grains can help regulate hormones and reduce oxidative stress. Supplements like CoQ10, vitamin D, zinc, and selenium may also support sperm and egg health. For women, vitex (chasteberry) and maca root are often used to support hormone balance. However, it’s best to work with a functional medicine or integrative practitioner to tailor a plan that suits your body.
Mental Health, Stress, and Fertility
It’s important not to overlook the role of stress and emotional health. Long COVID itself can be emotionally draining, and trying to conceive while coping with chronic symptoms may add another layer of anxiety. Cortisol, the body’s stress hormone, can interfere with reproductive hormones, delaying ovulation or affecting sperm quality. Mind-body practices like yoga, meditation, acupuncture, or breathwork can play a key role in rebalancing the nervous system and supporting overall fertility.
Experimental and Emerging Therapies
There’s also growing interest in Low Dose Naltrexone (LDN) and peptide therapies to modulate immune response and reduce inflammation in Long COVID cases. While not yet mainstream for fertility, these approaches are being explored in autoimmune infertility and may offer future potential. IV nutrient therapy, red light therapy, and herbal adaptogens like ashwagandha and rhodiola are also being studied for post-viral recovery and hormonal balance. Always consult a knowledgeable provider before starting experimental treatments.
Final Thoughts
The link between Long COVID and fertility is a complex and evolving field. While much remains to be understood, it’s clear that the virus can have lingering effects on reproductive health. The good news? Many of these effects may be temporary, and there are both conventional and holistic ways to support your fertility during recovery. Staying informed, advocating for your health, and working with compassionate professionals can make all the difference on this journey.
📩 Sign up for updates on Long COVID research and fertility support.